Kheradpisheh Z, Mirzaei M, Mahvi AH, Mokhtari M, Azizi R, Fallahzadeh H, Ehrampoush MH.
Journal Name: Nature | Scientific Reports
Publish Date: 02-08-2018
Volume/Page: 8(1):2674.
Abstract
Background
Artificial neural networks (ANNs) and adaptive neural-fuzzy Inference system (ANFIS) are the best solutions to finding the correlation between some water parameters and human hormones. The correlation between thyroid stimulating hormone (TSH) and drinking water fluoride studied by ANNS and ANFIS models in Yazd city.
Method
In this study, eighty people with thyroid gland disorder and 213 healthy people invited. Their thyroid hormones and fluoride drinking water analyzed.
Results
The result of ANFIS showed R2 = 0.81 for test and R2 = 0.85 for train in all cases and controls data. This results were R2 = 0.73 and R2 = 0.81 for ANNs respectively.
Conclusion
This models can be used as an alternative for show correlation between Drinking Water Fluoride and TSH Hormone and R2 = 0.85 gained from ANFIS was the best.
Keywords
Background
Fluoride, an anion of fluorine (halogen) is found in water. It has beneficial effects on teeth and bones at low concentrations but excessive exposure to fluoride has adverse effects [1, 2, 3, 4, 5, 6, 7, 8, 9, 10]. There are ways to get fluoride, but water is the most important [11, 12, 13, 14]. There are methods to remove fluoride from water that have been reported by researchers [15, 16, 17, 18]. Peckham (2014a; 2015b) stated that fluoride intake of more than 0.01 mg/kg body weight/day impacts thyroid gland function because it has adverse effects on iodine. Since children drink less water than adults, 0.8 mg/L is recommended by the European Union Scientific Committee on Health and Environmental Risk [5, 6]. Iran’s recommended level of fluoride in drinking water is 0.5–1.5 8 mg/L based on WHO Guidelines for drinking-water quality [19]. Dey and Giri (2016) found that excessive exposure to fluoride caused increase thyroid-stimulating hormone (TSH) and increase T3 and T4 hormones especially in people who do not consume enough iodine, therefore causing hypothyroidism [2]. They illustrated that consuming 20 mg/L sodium fluoride per day by rats repressed the production of nucleic acids and Triiodothyronine (T3), thyroxin (T4) hormones and change the activities of some metabolic enzyme such as: K (+) – Na (+) -ATPase, thyroid peroxidase, and 5, 5′-deiodinase [2]. Rastogi and Monika (2014) said that T3 and T4 are two hormones significant for the production of proteins to adjust body temperature which generates total energy, regulate the thyroid gland and controls human body metabolism [20]. Researchers have reported that thyroid dysfunction is a low thyroid production (hypothyroidism) or excessive production of thyroid hormone (hyperthyroidism) [21, 22, 23, 24, 25, 26]. Diagnosis of thyroid disease carried out by blood tests include the TSH, T4 test [22, 23, 27]. Governments are responsible for researching on the health challenges of its people due to reduced or excessive fluoride exposure [2]. Nowadays, computer technology and information have been developed in the sciences [28]. Therefore, artificial neural networks (ANNs) and adaptive neural-fuzzy Inference system (ANFIS) are the best solutions to finding the correlation between some water parameters and human hormones. ANNs are used for recognition, prediction, optimization, associative memory, and control [28]. ANNs have many advantages such as, flexible modeling structure for large data sets and highly accurate results that support clinical decision-making [29, 30, 31]. ANNs model was applied by some researchers in the diagnosis of thyroid disease [20, 21, 22, 24, 28, 48, and, 32, 33] and other diseases including diagnosis of tuberculosis [34], schizophrenia [36], anemia in children [37], heart disease [38] and, predicting prostate cancer [35]. Also, ANNS have been used by Lahner et al. (2008) in the recognition of the presence of thyroid disease in patients with atrophic body gastritis [39]. The aim of this study was to apply ANNS and ANFIS in modeling thyroid stimulating hormone (TSH) versus drinking water fluoride in Yazd city.
Methods
Study area, sample size, hormones analyze
The main source of drinking water in Yazd city is surface water and well resources in different seasons; thus, differences in fluoride concentration are bound to exist. Yazd city is the driest residential area in Iran [40]. Kheradpisheh et al. (2016) found that the mean ± SD of drinking water fluoride is 0.5 mg/L ± 0.27 in this area [3]. This nested case and control study selected cases and controls from Yazd Healthy Study (YaHS) which is a prospective cohort study. YaHS was conducted on ten thousand people aged 20 to 70 years in 2014 _ 2015. Details of Yazd Health Study has been published elsewhere [49]. The cluster sampling method was used in selecting cases with thyroid disease and medicine was not utilized. Control samples were participants with no thyroid disease aged 20 _ 60 years old. Eighty cases and 213 controls were selected. Informed consent was sought and obtained from the subjects upon which thyroid hormones test was conducted. Thyroid hormone analysis was carried out in Yazd Central Laboratory.
Drinking water fluoride study
Drinking water fluoride concentration was determined by SPADANS method number 8029 as described by Standard Methods for the Examination of Water and Wastewater [41]. All devices and reagents used in this study were obtained from HACH, Germany.
Application of ANNS and ANFIS model
The Neural Network Toolbox of Matlab© R2011a was used to create, train, and test data from ANNS and ANFIS model. Data were normalized. Inputs contained 268 out of every three T3, T4, and F from total cases and controls. Outputs were 268 out of TSH. Train GD, train GDA, train GDX, and train SCG, train LM were used as network training function, and R2, RMSE, NRMSE were obtained from test plot model and Test Scatter model for TSH hormone and also to train all cases and control data by ANNS and ANFIS model. The abbreviations are explained in Abbreviations list in this text. The training was achieved by a back propagation method after setting network properties and raining parameters. Back propagation method has been used on some research as Aktan et al. (2016); Boyacioglu et al. (2010); Rezaei Kahkha et al. (2016); Razia et al. (2016); Svalina et al. (2013) [22, 42, 43, 44, 45]. The network was tested with thyroid hormones data collected from cases and controls and measured drinking water fluoride concentration.
Data Availability
Please contact the author for data requests.
Results
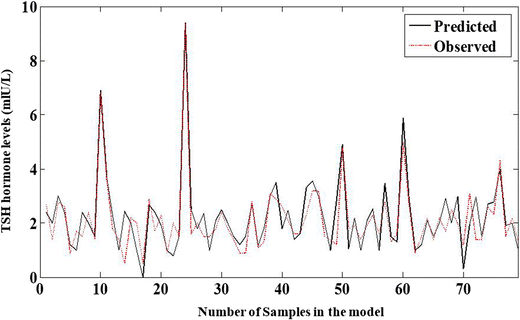
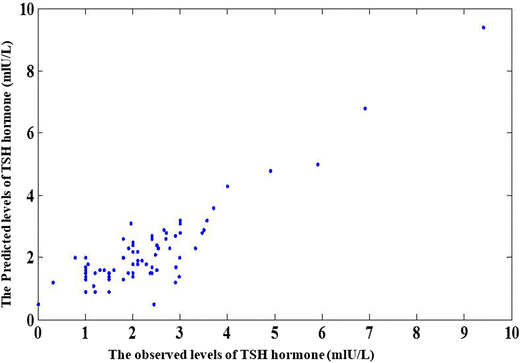
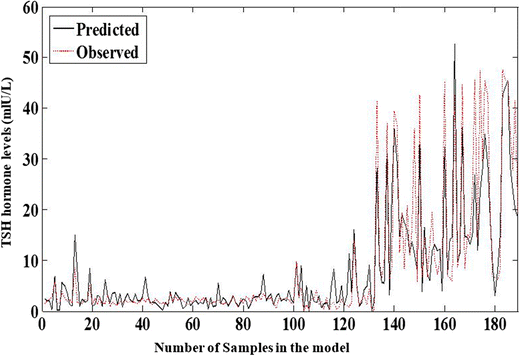
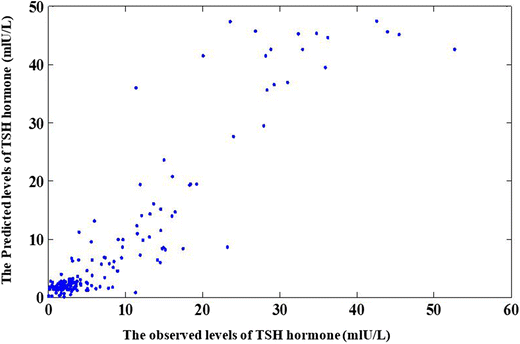
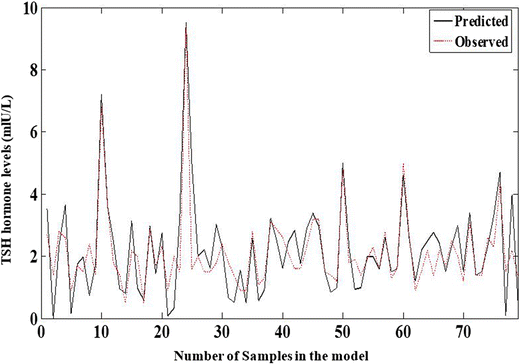
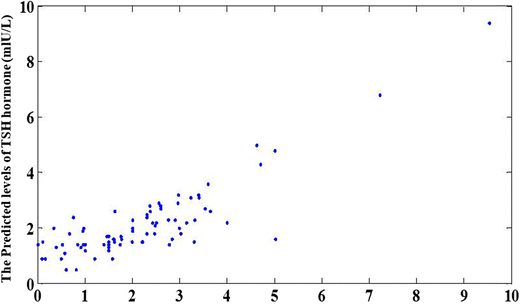
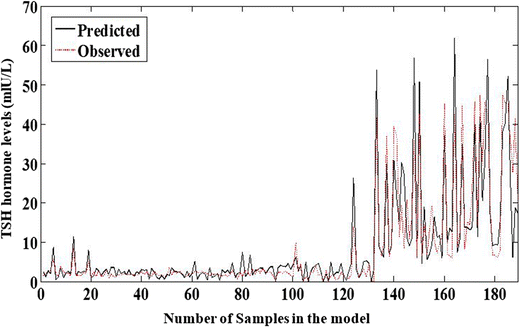
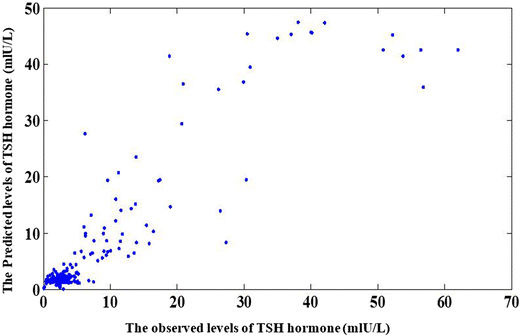
The main goal of this paper was to apply ANNS and ANFIS Models for TSH Hormone modeling versus Drinking Water Fluoride in Yazd city. In this study, R square, RMSE, and NRMSE were calculated for observed and predicted data in ANNS and ANFIS models. Figures 1 and 2 indicate the correlation diagram for Test Plot model and Test Scatter model for TSH hormone in all cases and control data by ANFIS Model. The results were: R2 = 0.81, RMSE = 0.6, NRMSE = 6.4. Figures 3 and 4 show the train plot model and train scatter model results for TSH hormone in all cases and controls data by ANFIS Model. The result were: R2 = 0.85, RMSE = 4.8, NRMSE = 9.3. The back propagation learning algorithm was used to minimize system error between real output and target output. The number of hidden layer are achieved by trial and error method in the ANNS and ANFIS Models. Figures 5 and 6 show the test plot model and test scatter model results for TSH hormone in all cases and control data by ANNS Model. The results were: R2 = 0.73, RMSE = 0.8, NRMSE = 8.4. Figures 7 and 8 show the train plot model and results for TSH hormone in all cases and controls data by ANNS Model. The results were: R2 = 0.81, RMSE = 5.15, NRMSE = 9.5.The number of Epoch was1000, the number of hidden layer was 9, the number of train algorithm was 5 contain: train GD, train GDA, train GDX, train SCG, and train LM for ANNS and ANFIS models. The best train algorithm was train LM. 268 out of 293 (80 cases and 213 controls) cases were used in the ANNS and ANFIS models as the age was not within our desirable range or the results of all three hormones were not acceptable. Inputs were 268 out of every three T3, T4, and F from total cases and controls. Outputs were 268 out of TSH. Test Inputs were 79 out of every three T3, T4, and F from total cases and control. Test Outputs were 79 out of TSH. Train Inputs were 189 out of every three T3, T4, and F from total cases and control. Outputs were 189 out of TSH.
Fig. 1
Test Plot model for TSH hormone in all data (Cases and controls) by ANFIS. R2 = 0.81, RMSE = 0.6, NRMSE = 6.4
Fig. 2
Test Scatter model for TSH hormone in all data (Cases and controls) by ANFIS.R2 = 0.81, RMSE = 0.6, NRMSE = 6.4
Fig. 3
Train Plot model for TSH hormone in all data (Cases and controls) by ANFIS. R2 = 0.85, RMSE = 4.8, NRMSE = 9.3
Fig. 4
Train Scatter model for TSH hormone in all data (Cases and controls) by ANFIS. R2 = 0.85, RMSE = 4.8, NRMSE = 9.3
Fig. 5
Test Plot model for TSH hormone in all data (Cases and controls) by ANNS. R2 = 0.73, RMSE = 0.8, NRMSE = 8.4
Fig. 6
Test Scatter model for TSH hormone in all data (Cases and controls) by ANNS. R2 = 0.73, RMSE = 0.8, NRMSE = 8.4
Fig. 7
Train Plot model for TSH hormone in all data (Cases and controls) by ANNS. R2 = 0.81, RMSE = 5.15, NRMSE = 9.5
Fig. 8
Train Scatter model for TSH hormone in all data (Cases and controls) by ANNS. R2 = 0.81, RMSE = 5.15, NRMSE = 9.5
Discussion
Results show that outcomes of ANNs and ANFIS models are in good agreement with experimental data; this indicates that ANNs and ANFIS models can be used as an alternative for the determination of correlation between TSH hormone and drinking water fluoride. R2 = 0.85 was the best value obtained from the ANFIS model. In this paper, by selecting 9 neurons in the hidden layer, we can reach 81% classification accuracy for thyroid disease by ANNs and 85% by ANFIS. This paper presents ANFIS model as an assistance system for the determination of correlation between TSH and fluoride. This model used drinking water fluoride, an environmental factor, as an input data and TSH hormone value as output of the model which determine hypothyroidism like an endocrinologist expert. To determine the correlation between TSH hormone and how other environmental factors play an important role in the prevention of hypothyroidism especially in places with high fluoride in the water. In spite of the fact that, many successful studies using neural networks and ANFIS for classification including medical diagnosis like: (Adeli and Neshat (2010); Caturegli et al. (2014); Emin Aktan et al. (2016); Omitek et al., 2013); Prerana et al. (2015); Rastogi and Monika (2014); Saylam et al. (2013); Soleimanian et al. (2013) [20, 21, 22, 24, 28, 33, 46, 48], But in this paper, we presented the correlation between disease and drinking water factor that we think is more important especially in the study area. The results clearly show that neural networks as traditional statistical methods can estimate these correlations.
As Galletti and Joyet (1958) pointed out, fluoride was used to treat hyperthyroidism in South America and Europe in 19 decades. Iodine is used by the thyroid gland to make T3 and T4 hormones. When iodine is low in the body, other available halogens such as bromine, chlorine, and fluorine will be absorbed into and block the thyroid gland [47]. In areas that experience excess fluoride, especially from water, low iodine levels in the body can cause fluoride uptake into the thyroid gland. Thus, to help our thyroid function, we must consider limiting fluoride exposure and adding iodine to our diet [47]. As mentioned by Basha et al. (2011) and Dey and Giri (2016), fluoride can block the iodine receptors in the thyroid gland therefore, we are suggest a study can be done on using pure treated drinking water by hypothyroidism when they are treated by medication. The thyroid gland is the most sensitive tissue in the body to fluoride [2]. Basha et al. (2011) and Dey and Giri (2016) stated that TSH hormone as well as T3 and T4 hormones decreased due to excess fluoride concentration and thus cause hypothyroidism in some populations [1, 2]. This paper showed this reality that the value of TSH hormone increased by increasing water fluoride concentration. Our results are in line with those of other researches such as Basha et al. (2011) and Dey and Giri (2016).
Conclusion
Essentially, it means that the ANNS and ANFIS methods can be used to modeling thyroid stimulating hormone (TSH) versus drinking water fluoride. The proposed method in this paper can be a solution to increase the performance of ANNS and ANFIS. Therefore, it can be generalized to determine other factors that affect TSH hormone by models. For further studies and investigation, we propose using sex, age, physical conditions, environmental factors especially drinking water etc., as effective factors in thyroid diagnosis.
Declarations
Acknowledgements
We acknowledge Yazd Healthy Study participants who gave us their time and drinking water samples.
Funding
This research was supported by Yazd University of Medical Sciences.
Author contributions
ZKH and MHE was the main investigator, collected the data, MM, MM and AHM supervised the study. MK and RA and HF were advisors of the study. All authors read and approved the final manuscript.
Compliance with ethical standards
This study is Compliance with Ethical Standards. This study funded by Environmental Science and Technology Research Center, Department of Environmental Health Engineering, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
Ethical approval
Case and control people choses with their consent and have been informed about study and they invited for Thyroid hormones test. Their thyroid hormones analyze in Yazd Central Laboratory.
Competing interests
The authors declare that they have no competing interests.
References
- Basha PM, Rai P, Begum S. Fluoride toxicity and status of serum thyroid hormones, brain histopathology, and learning memory in rats: a multigenerational assessment. Biol Trace Elem Res. 2011;144:1083–94.View ArticleGoogle Scholar
- Dey S, Giri B. Fluoride fact on human health and health problems: a review. Med Clin Rev. 2016;2(1):11. https://doi.org/10.21767/2471-299X.100011.View ArticleGoogle Scholar
- KheradPisheh Z, Ehrampoush MH, Montazeri A, Mirzaei M, Mokhtari M, Mahvi AH. Fluoride in drinking water in 31 provinces of Iran. Expo Health. 2016;8:465–74. https://doi.org/10.1007/s12403-016-0204-z.View ArticleGoogle Scholar
- Lennon M A, Whelton H, O’Mullane D, Ekstrand J. Fluoride. Rolling revision of the WHO guidelines for drinking-water quality. World Health Organization. 2004.Google Scholar
- Peckham S, Awofeso N. Water fluoridation: a critical review of the physiological effects of ingested fluoride as a public health intervention. Sci World J. 2014;2014:293019.View ArticleGoogle Scholar
- Peckham S, Lowery D, Spencer S. Are fluoride levels in drinking water associated with hypothyroidism prevalence in England? A large observational study of GP practice data and fluoride levels in drinking water. J Epidemiol Community Health. 2015;0:1–6. https://doi.org/10.1136/jech-2014-204971. Google Scholar
- Rahmani A, Rahmani K, Dobaradaran S, Mahvi AH. Hamadjani RM, Rahmani H. Child dental caries in relation to fluoride and some inorganic constituents in drinking water in Arsanjan, Iran. Fluoride. 2010;43:179–86.Google Scholar
- Dobaradaran S, Mahvi AH, Dehdashti S, Abadi DRV. Drinking water fluoride and child dental caries in Dashtestan, Iran. Fluoride. 2008;41:220–6.Google Scholar
- Mahvi AH, Zazoli MA, Younecian M, Nicpour B, Babapour A. Survey of fluoride concentration in drinking water sources and prevalence of DMFT in the 12 years old students in Behshar City. J Med Sci. 2006;6:658–61.View ArticleGoogle Scholar
- Rahmani A, Rahmani K, Mahvi AH, Usefie M. Drinking water fluoride and child dental caries in Noorabademamasani, Iran. Fluoride. 2010;43:187–93.Google Scholar
- Dobaradaran S, Mahvi AH, Dehdashti S. Fluoride content of bottled drinking water available in Iran. Fluoride. 2008;41:93–4.Google Scholar
- Dobaradaran S, Mahvi AH, Dehdashti S, Dobaradaran S, Shoara R. Correlation of fluoride with some inorganic constituents in groundwater of Dashtestan, Iran. Fluoride. 2008;42:50–3.Google Scholar
- Mahvi AH, Zazoli MA, Younecian M, Esfandiari Y. Fluoride content of Iranian black tea and tea liquor. Fluoride. 2006;39:266–8.Google Scholar
- Nouri J, Mahvi AH, Babaei A, Ahmadpour E. Regional pattern distribution of groundwater fluoride in the shush aquifer of Khuzestan County, Iran. Fluoride. 2006;39:321–5.Google Scholar
- Zazouli MA, Mahvi AH, Dobaradaran S, Barafrashtehpour M, Mahdavi Y, Balarak D. Adsorption of fluoride from aqueous solution by modified Azolla filiculoides. Fluoride. 2014;47:349–58.Google Scholar
- Bazrafshan E, Ownagh KA, Mahvi AH. Application of electrocoagulation process using Iron and aluminum electrodes for fluoride removal from aqueous environment. E-J Chem. 2012;9:2297–308.View ArticleGoogle Scholar
- Boldaji MR, Mahvi AH, Dobaradaran S, Hosseini SS. Evaluating the effectiveness of a hybrid sorbent resin in removing fluoride from water. Int J Environ Sci Technol. 2009;6:629–32.View ArticleGoogle Scholar
- Dobaradaran S, Fazelinia F, Mahvi AH, Hosseini SS. Particulate airborne fluoride from an aluminium production plant in arak, Iran. Fluoride. 2009;42:228–32.Google Scholar
- World Health Organization. Guidelines for Drinking-water Quality; 2011. Fourth edition, ISBN 978 92 4 154815 1.Google Scholar
- Rastogi BA, Monika A. Study of neural network in diagnosis of thyroid. IJCTEE. 2014;4(3):13–6.Google Scholar
- Caturegli P, Remigis A, Rose NR. Hashimoto thyroiditis: clinical and diagnostic criteria. Autoimmun Rev. 2014;13:391–7.View ArticleGoogle Scholar
- Emin Aktan M, Akdogan E, Zengin N, Guney OF, Parlar RE. An artifitial neural network design for determination of Hashimoto’s thyroiditis sub- groups, CBU international on innovations in science and education. 2016:23-25, Prague, Czech Repablic WWW.CBUNI.CZ, WWW.JOURNALS.CZ
- Health Information. Endocrine Diseases. Hashimoto’s Disease. 2016. www.niddk.nih.gov/health-information/health-topics/endocrine/hashimotos-disease/16.03.2016.
- Omitek Z, Burda A, Wojcik W. The use of decision tree induction and artificial neural networks for automatic diagnosis of Hashimoto’s disease. Expert Syst Appl. 2013;40:6684–9.View ArticleGoogle Scholar
- Sundaram N M, Renupriya V. Artificial neural network classifiers for diagnosis of thyroid abnormalities. International conference on systems, science, control, communication, Eng Technol 2016: 206–211.Google Scholar
- Zhang GP, Berardi VL. An investigation of neural networks in thyroid function diagnosis. Health Care Manage Sci. 1998;1:29–37.View ArticleGoogle Scholar
- Ozyılmaz L, Yıldırım T. Diagnosis of thyroid disease using artificial neural network methods. In: Proceedings of ICONIP’02 9th international conference on neural information processing (Singapore: Orchid Country Club, 2002). 2002, p. 2033–2036.Google Scholar
- Soleimanian Gharehchopogh F, Molany M, Dabaghchi MF. Using artificial neural network in diagnosis of thyroid disease: a case study. IJCSA. 2013;3(4):49–61. https://doi.org/10.5121/ijcsa.2013.3405.Google Scholar
- Innocent PR, John RI, Garibaldi JM. Fuzzy methods for medical diagnosis. Appl Artif Intell. 2004;19(1):69–98.View ArticleGoogle Scholar
- Zarandi F, Zolnoori MH, Moin M, Heidarnejad HA. Fuzzy rule-based expert system for diagnosing asthma. Sharif University of Technology. Transaction E. Ind Eng. 2010;17(2):129–42. www.SID.ir Google Scholar
- Ghahazi MA, Zarandi F, Harirchian MH, Damirchi-Darasi SR. Fuzzy rule based expert system for diagnosis of multiple sclerosis. IEEE conference on Norbert wiener in the 21st century (21CW), Boston, MA. 2014: 1–5.Google Scholar
- Amrollahi Biyouki S, Türksen IB, Fazel Zarandi MH. Fuzzy rule-based expert system for diagnosis of thyroid disease. IEEE. International Conference on Fuzzy Systems. Computational Intelligence in Bioinformatics and Computational Biology (CIBCB). 2015 I.E. Conference. Niagara Falls, ON, Canada 19 October 2015.Google Scholar
- Saylam B, Keskek M, Ocak S, Akten AO, Tez M. Artificial neural network analysis for evaluating cancer risk in multinodular goiter. J Res Med Sci. 2013;18(7):554–7.Google Scholar
- Er O, Temurtas F, Tanrıkulu AÇ. Tuberculosis disease diagnosis using artificial neural networks. J Med Syst 2013. 2010;34(3):299–302. https://doi.org/10.1007/s10916-008-9241-x.Google Scholar
- Castanho MJP, Hernandes F, De Re AM, Rautenberg S, Billis A. Fuzzy expert system for predicting pathological stage of prostate cancer. Expert Syst Appl. 2013;40:466–70.View ArticleGoogle Scholar
- Takahashi M, Hayashi H, Watanabe Y. Diagnostic classification of schizophrenia by neural network analysis of blood-based gene expression signatures. Schizophr Res. 2010;119:210–8.View ArticleGoogle Scholar
- Kaya E, Aktan ME, Akdoğan E, Koru AT. Diagnosis of anemia in children via artificial neural network. IJISAE. 2015;3(1):24–7. www.atscience.org/IJISAE View ArticleGoogle Scholar
- Ebenezer O, Oyebade O, Oyedotun K, Helwan A. Neural network diagnosis of heart disease, Conference Paper 2015. https://doi.org/10.1109/ICABME.2015.7323241.
- Lahner E, Intraligi M, Buscema M, CentANNsi M, VANNsella L, Grossi E, et al. Artificial neural networks in the recognition of the presence of thyroid disease in patients with atrophic body gastritis. World J Gastroenterol. 2008;14(4):563–8.View ArticleGoogle Scholar
- Census of the Islamic Republic of Iran. Islamic Republic of Iran. Archived from the original (excel) on. 2011–11-11. 2006.Google Scholar
- Lenore S, Arnold E, Andrew D. Standard methods for the examination of water and wastewater, American public health association, American Water Works Association, water environment federation. The twentieth edition. 4500-F– D. SPADNS Method. 2005;20:140–3.Google Scholar
- Boyacioglu MA, Avci D. An adaptive network-based fuzzy inference system (ANFIS) for the prediction of stock market return: the case of the Istanbul stock exchange. Expert Syst Appl. 2010;37:7908–12.View ArticleGoogle Scholar
- Rezaei Kahkha MR, Piri J. Comparison of artificial neural network and neutral-fuzzy inference system for photo catalytic removal of reactive red dye. Tech J Engine App Sci. 2016;6(1):39–44.Google Scholar
- Razia SH, Narasinga Rao MR. Machine learning techniques for thyroid disease diagnosis – a review. Indian J Sci Technol. 2016;9(28) https://doi.org/10.17485/ijst/2016/v9i28/93705, July.
- Svalina L, Galzina V, Lujic R, Šimunovic G. An adaptive network-based fuzzy inference system (ANFIS) for the forecasting: the case of close price indices. Expert Syst Appl. 2013;40:6055–63.View ArticleGoogle Scholar
- Adeli A, Neshat M. A Fuzzy Expert System for Heart Disease Diagnosis in Proceedings of the International Multi Conference of Engineers and Computer Scientists, Hong Kong. March 17–19 2010; 1Hong Kong.Google Scholar
- Galletti P, Joyet G. Effect of fluorine on thyroidal iodine metabolism in hyperthyroidism. J Clin Endocrinol. 1958;18(10):1102–10.View ArticleGoogle Scholar
- Prerana SP, Taneja K. Predictive Data Mining for Diagnosis of Thyroid Disease using Neural Network. Int J Res Manage Sci Technol. 2015;3(2):75–80. Available at www.ijrmst.org Google Scholar
- Mirzaei, M., Salehi-Abargouei, A., Mirzaei, M., Mohsenpour, M.A. Cohort profile: the Yazd health study (YaHS): a population-based study of adults aged 20–70 years (study design and baseline population data). Int J Epidemiol 1–10 (2017). https://doi.org/10.1093/ije/dyx231.